All pharmacy benefit partners use a regularly updated list of medications called a formulary to inform participants which prescriptions are considered preventive (and often free), preferred or requiring special authorization to fill. You always may ask your doctor or pharmacist whether a lower-cost alternative prescription is available.
Generic medications are proven to hold the same potency and results as brand equivalents. Whenever they’re available, generic medications are substituted for brand medicines unless your doctor indicates “Dispense as Written” on the prescription. If either you or your doctor requests a brand-name medicine when a generic is available, you are responsible for paying the cost difference.
Step therapy is a strategy a doctor may use when a patient starts taking certain medications. Monitoring the patient’s results with the medication before changing the dose or the prescription may be necessary, especially if a medication could be costly or cause undesirable side effects. Each patient’s situation is unique, so it’s a good idea to discuss each new prescription with your doctor or pharmacist before moving forward.
If you’re enrolled in the CDHP, prescriptions are subject to the medical plan deductible, meaning that you pay the full cost of non-preventive medications until you reach the annual deductible. Costs incurred while using your medical coverage, including but not limited to prescriptions, count toward the deductible. You can use your Health Savings Account to pay for prescriptions. Preventive generic medications are $0 under the CDHP.
Maintenance medications are prescriptions intended to be taken regularly for more than 90 days. You may receive up to two 30-day refills at a network retail pharmacy, but you must request a 90-day prescription if applicable. Then, those medications are filled via mail order. Otherwise, you are responsible for the full cost of the medication.
If a medication you’ve been taking becomes unavailable for any reason, contact Optum right away. Be sure to describe the condition(s) for which you were prescribed the medication. If you experience a delay in getting the prescription you need through Optum, you may be able to pay out of pocket for a short-term supply of certain medications using your pharmacy’s prescription discount program. Discuss the situation with your pharmacist to find out if your prescription is eligible.
Having a single pharmacy benefits partner ensures that everyone covered by an Asurion medical plan who has a medical condition that requires maintenance medication gets the high-quality care we expect. Optum is integrated with Livongo for diabetes and Hello Heart for hypertension care. For these patients and others with serious health concerns, we want to deliver an individualized care plan. This includes but isn’t limited to a concierge service to schedule and coordinate medical appointments and, if desired, to help monitor prescription adherence so patients can avoid detrimental health effects.
Heads up! You are leaving the ABC InfoShare. Unless you’re on the Asurion network, you’ll need your username and password to access Asurion Benefits Central at asurion.benefitsnow.com. Only current Asurion employees may log in.
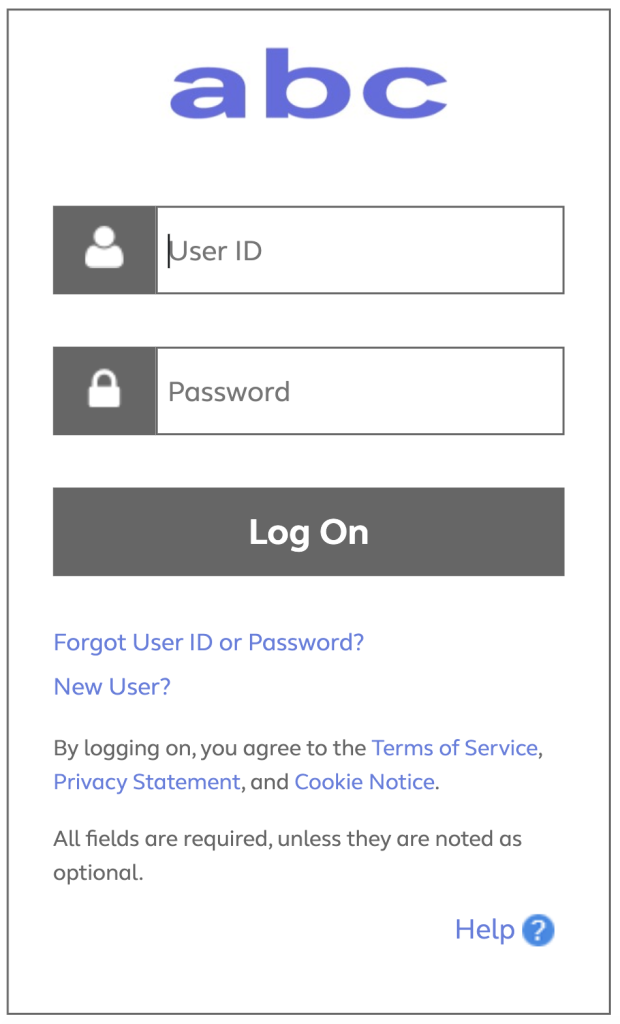
If you don’t have the required log-in details, select Forgot User ID or Password? and follow the prompts. If this is your first visit to Asurion Benefits Central, click New User?
Questions: Call 844.968.6278.
Register in Asurion Learning for the meeting you’d like to attend. After registering, you’ll receive a confirmation email containing information about joining the meeting.
No events found.

Text “Benefits” to 67426 to have a link sent to your phone. Then, click the link to download the Alight Mobile app so you can access all the functions of the ABC on the go. (You’ll need to set your “Primary Phone” in Workday as your mobile number for full functionality.)